SPATH

Two recent articles in the Telegraph: NHS Scotland plans to ‘fast-track irreversible surgery for trans patients’ and Women’s health clinics could be renamed to avoid upsetting trans patients have focused on a report called the Scottish Pathway for Trans Healthcare (SPATH). This was one of several documents provided by NHS Greater Glasgow and Clyde in response to our Freedom of Information request, and details the proposed national treatment guidelines for transgender patients. NHS Scotland have said the guidelines are due to be sent to the Scottish Government for final approval.
SPATH, September 2022
Numerous documents are embedded in SPATH which are given separately here:
– Assessment example journeys
– GS prison model
– GS prison model Appendix 1
– Endocrine and fertility preservation guidance
– Masculinising treatment FINAL
– Feminising treatment FINAL
– Trans voice & communication leaflet
– Facial hair removal guidelines
– Letter re provision of wigs
– YP gender service assessment proforma
– GRP children’s and YP age and stage
– Recommendations for GRP YP subgroup
Other documents included in the FOI:
SPATH Update, April 2022
SPATH Initial Briefing, February 2022
Sandyford GIC’s response to ICD-11 reclassification of gender dysphoria
The guidance is the end result of a request from the Chief Medical Officer in July 2021 to review the current Gender Reassignment Protocol and update it in line with best practice, taking into account the latest World Professional Association of Transgender Health (WPATH) guidelines, and the recent reclassification in ICD-11 of the mental health condition of gender dysphoria to a sexual health condition of gender incongruence.
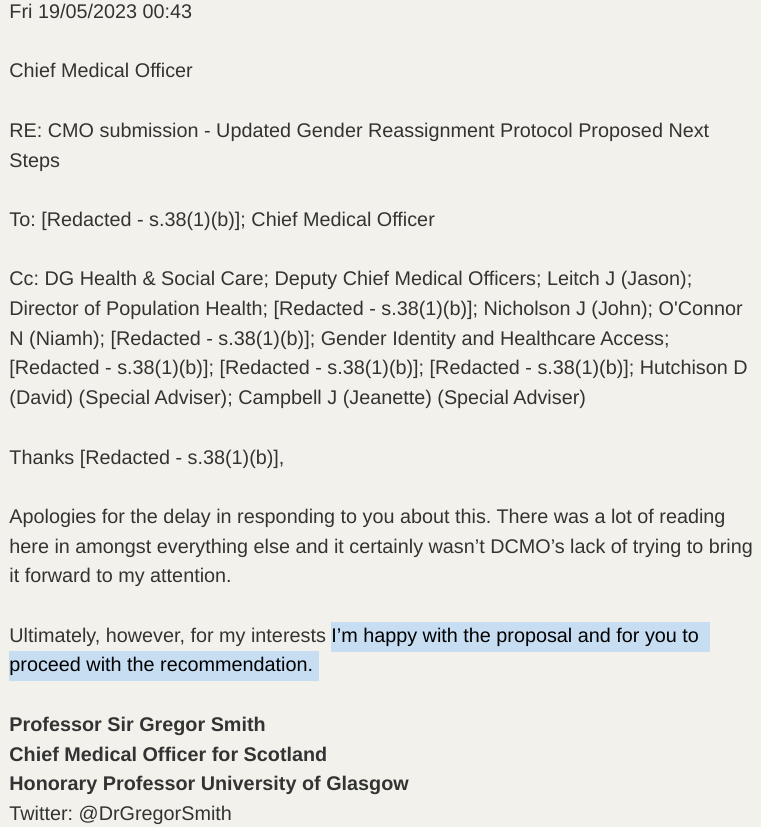
As expected from a treatment protocol heavily based on the discredited WPATH standards of care, there are numerous concerns with SPATH, including the following:
‘Barriers’ to surgery should be removed with surgery seen as a preventative measure rather than to cure distress:
- No psychiatric diagnosis of gender dysphoria, patient assessed only for readiness for the hormone or surgical procedure requested.
- Only one opinion needed to refer patient for surgery except in ‘complex’ cases.
- Counselling or psychotherapy “not a prerequisite” before irreversible surgeries.
- Specialist GPs, rather than gender identity specialists, should be able to refer patients for surgery.
- Senior clinicians or psychiatrists treating a patient’s complex mental health problems barred from involvement in assessing readiness for surgery.
- More surgeries recommended by WPATH may become available on Scottish NHS in future (eg. voice feminisation surgery).
- Patients placed on medical pathways after brief assessment as lower level interventions like voice therapy/wigs are deemed “extremely low risk”.
GPs should be able to prescribe hormones and non-specialists to assess patients:
- Family doctors should be able to sign “shared care agreements” with gender clinics to prescribe drugs as part of an “enhanced service”.
- Backs a pilot project for those “self-sourcing” their own hormones to get priority referrals to clinics, despite admitting this could incentivise use.
- A “safer alternative” should be provided by GPs where patients are self-prescribing.
- A wide variety of health professionals can develop competencies to carry out assessments of readiness for gender affirming healthcare, including doctors working in primary or secondary care (such as GPs with special interest, psychiatrists, sexual health specialists, and endocrinologists), nurse practitioners, psychologists, and allied health professionals (such as occupational therapists).
Services for children to continue with “affirming” approach despite Cass review:
- A long-term approach to treating children will have a “trans affirmative approach” (Cass warned about this).
- Literature to be developed for children, including under 13s, telling them about the “importance of gender affirming care”.
- Opens door to GPs prescribing puberty blockers, saying role of primary care “to deal with treatment following assessment” should be considered, “reducing the need for specialist clinicians”.
- Hormone/puberty blockers continue to be prescribed despite Cass’s early findings of scant evidence for their use, only to be reviewed 12-18 months after SPATH published.
- Fund partnership work with third sector organisations to provide patient support, including group work and befriending. Badged as from the NHS to “provide credibility”.
- No consideration of care for detransitioners.
NHS Scotland should “move away” from “gendered healthcare”:
- Report says “systems within NHS Scotland need to allow for increasing gender identities for patients, specifically including non-binary identities. This should be done as part of a general move away from gendered healthcare.”
- Claims transmen may feel uncomfortable seeking contraception or smear tests when the services “target audience” is incongruent to their gender identity, such as a “women health clinic”.
- “If clinically appropriate, laboratory reference ranges should be decoupled from gender markers and instead be relevant to the individual”.
- Suggestion of “inclusive” signage, forms and leaflets, and appropriate staff training.
- Where CHI number is changed, responsibility placed on the patient to decide when it is appropriate to disclose their sex to “ensure patient safety” or for “determining appropriate care”.
Update 31 July 2023:
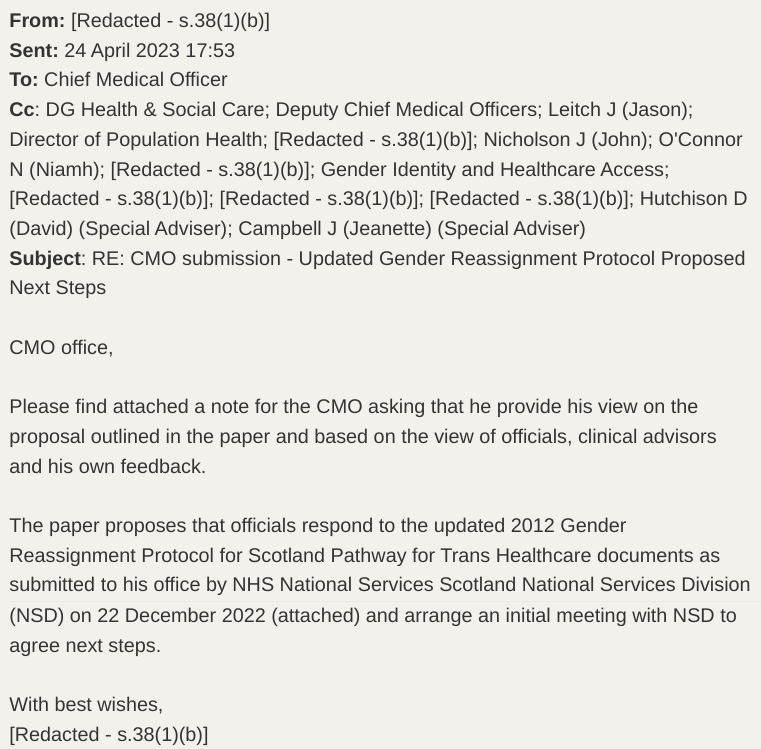
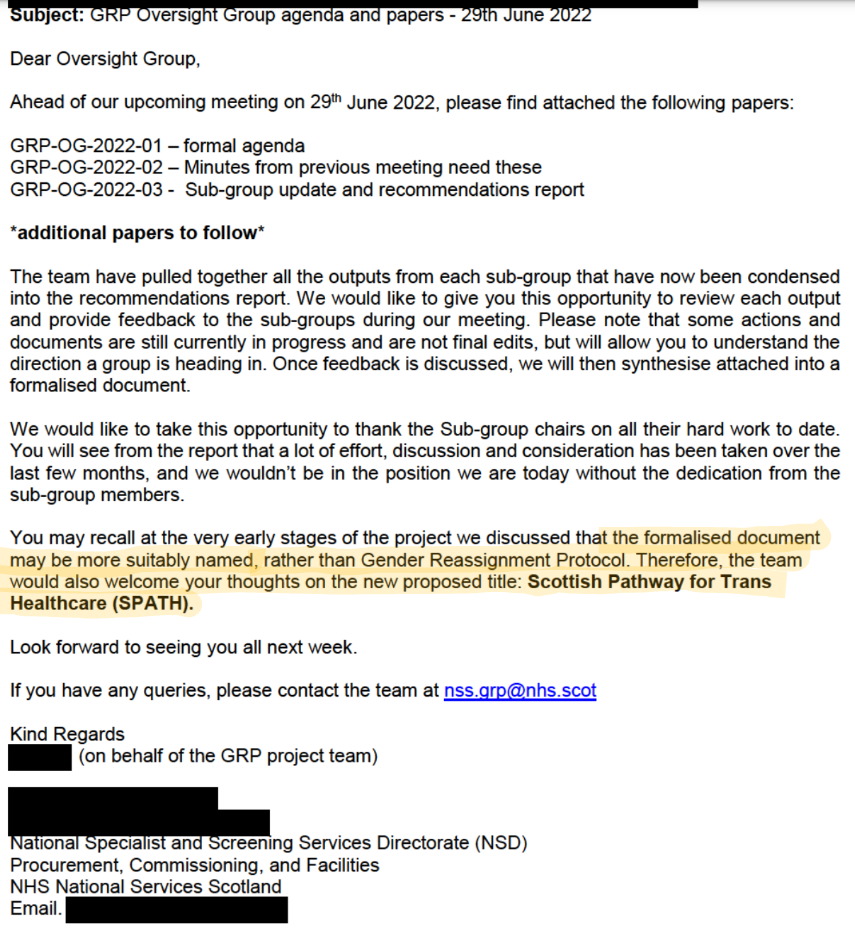
A Freedom of Information response (see attachment E) revealed that the Chief Medical Officer has approved SPATH.
Update 03 August 2023:
Following this tweet, the Scottish Daily Express wrote an article about the Chief Medical Officer giving his approval to SPATH in which the Scottish Government gave the following comment:
“The paper referred to is not an update of the 2012 Gender Reassignment Protocol for Scotland. Any suggestion this or a final document has been “approved” by the Chief Medical Officer is incorrect.
The Chief Medical Officer has received a revised and updated Protocol from NHS National Services Scotland. This is being carefully considered prior to any future publication.”
The paper referred to dates from June 2022. It is one paper of many, which will inform a final document, and includes preliminary recommendations which were to be further considered prior to drafting a revised Protocol.”
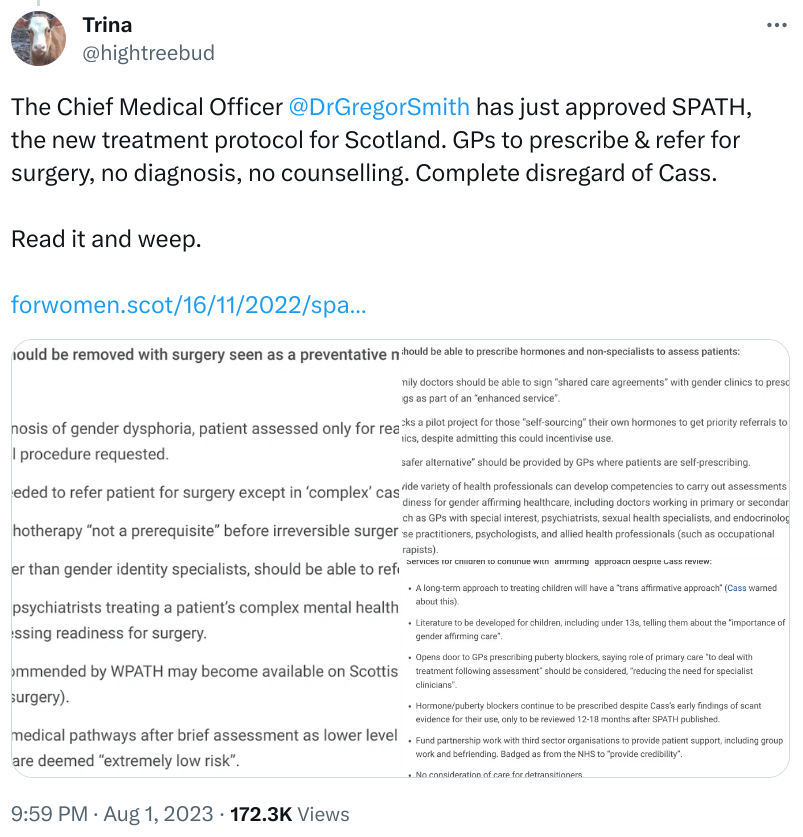
We found this comment very odd. The paper referred to in the newspaper article is SPATH and as the following email shows (released as part of our original FOI) there was a proposal to rename the updated Gender Reassignment Protocol as SPATH. This FOI response confirms the new title was adopted on 6th June 2023.
It is very clear that SPATH is the update of the Gender Reassignment Protocol and this is further confirmed in the original email NSS sent to the CMO on 20th December 2022 which refers to the CMO’s 2021 request to refresh the GRP and attached the “updated document now titled the NHS Scotland Pathway for Trans Healthcare”.
The document properties of the SPATH we received show it was created on 6th September 2022 – not June, as claimed by the Government spokesperson.
The only question that remains is what amendments were made to this document before it was sent to the CMO in December 2022. Given the timeframe, any changes are unlikely to be substantial and the minutes of the Government’s National Gender Identity Healthcare Reference Group suggests minor editing and compiling changes. We can’t know for sure because a FOI request for the exact version sent to the CMO was denied, citing Section 27(1) of FOISA: the information is being withheld because it is due to be published shortly.
From his email reply on the 19th May 2023 the CMO was clearly content with the updated GRP/SPATH proposals and gave the go ahead to proceed with the recommendations therein.
We are fascinated to know why the Government spokesperson thinks the GRP is still under consideration by the CMO or that SPATH is only a paper to feed into the still to be written GRP – particularly when the updated GRP, retitled as the NHS Scotland Trans Healthcare Pathway, was due to be published on 6th June 2023. This did not happen and we await NSS’s response to a FOI request as to the reasons why, and if there is a new publication date planned.
For an update that has been a substantial piece of work, taking in excess of two years to complete and with the reported input of over 60 experts, we cannot help but wonder why the Scottish Government seems to be backtracking from it at the rate of 100mph. We can only hope it is in response to NHS England announcing on 27th July 2023 that there is insufficient evidence to support the safety, clinical effectiveness and cost effectiveness of Puberty Suppressing Hormones and they will no longer be prescribed outside a research programme.
They have also justified why they are not aligning with WPATH with “NHS England commissions treatment based on evidence of clinical effectiveness, cost effectiveness and safety. WPATH standards of care do not determine clinical commissioning decision for the NHS.”
With the same information available to NHS Scotland it is unclear why their updated GRP/SPATH has taken the opposite stance to NHS England by continuing to prescribe puberty suppressing hormones and following WPATH guidance. We hope the realisation is dawning that they look like dangerous fools prepared to risk the health of Scottish children and, as such, the SPATH document will never see the light of day.