Sandyford
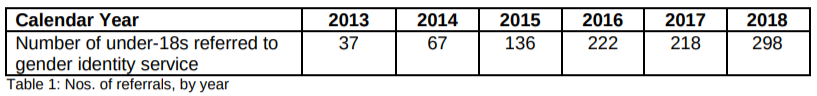
A recent Freedom of Information response, as reported in today’s The Times, has revealed that referrals for Scottish children to the Sandyford Young People’s Gender Service have risen by an unprecedented 705% since 2013, in comparison to a rise of 438% for the Tavistock in London over the same time period.
As of 2018 there are also an additional 470 children (aged 16.5 years or younger) on a waiting list for a first appointment.
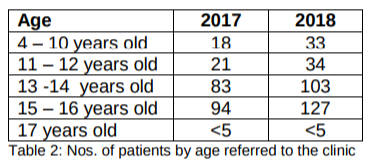
The age group with the largest number of referrals is that of 15-16 year olds, for whom referrals have increased by 35% in the year from 2017 to 2018. Worryingly the number of much younger children referred has rocketed with a rise of 62% for 11-12 year olds, and a startling rise of 83% for 4-10 year olds between 2017 and 2018.
This last figure is particularly worrying as, according to Sandyford’s own criteria, such young children should not even be in their system:
- Sandyford provide counselling and support services for young people aged 13-17
- “The focus of the Young Person’s Service is to support young people (and their families) experiencing gender dysphoria who are either entering puberty or are progressing with puberty. The Service has less of a role with pre-pubertal children who are supported by more local resources; this may include input from local Child and Adolescent Mental Health Services.” (see page 36)
The FoI asked for the numbers and ages of children when they were first prescribed puberty blockers. This information is not available as it is not held in a central database. We are concerned that there does not appear to be overall monitoring of the number of children accessing this controversial medical treatment.
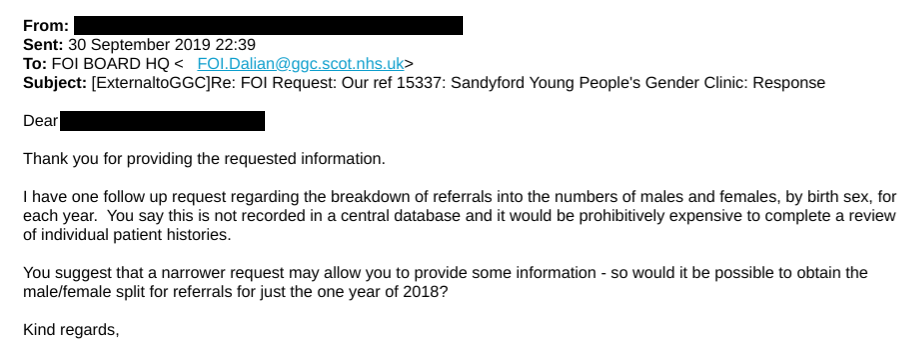
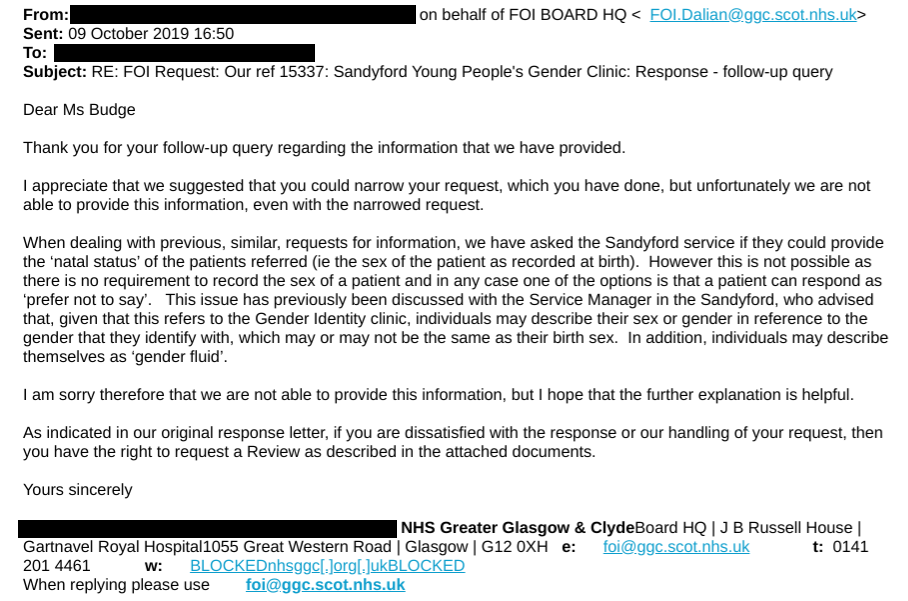
Nor is the split in referrals between male and female children being monitored. A follow up request asked if the referrals for just the last year could be broken down into numbers of males and females, but apparently this is not possible as there is no requirement to even record the sex of a patient on case notes, and the patient may choose to give their identified sex or prefer not to say. It seems ludicrous that medical notes may not accurately record a patient’s sex and we can only wonder how this potentially affects treatment.
Transgendertrend has analysed the continuing increase in the number of girls referred to Tavistock, “In less than a decade there has been a 1,460% increase in referrals of boys and a staggering 5,337% increase in girls”, with girls now making up 74% of the total referrals last year. The underlying causes of this significant change remain unknown, but caused enough concern to prompt the then Women’s Minister, Penny Mordaunt, to initiate an investigation.
This situation seems to be mirrored throughout many western countries and is likely to be similar in Scotland. However, the lack of sex-disaggregated data collection prevents the problem from even being identified, never mind any steps taken to investigate or address it. We intend raising this with the Scottish Government’s newly established working group on sex and gender in data.
In 2015 Dr David Gerber from Sandyford said “with no specific treatment available the usual approach was ‘watchful waiting’”, yet by 2017 Sandyford have clearly followed Tavistock’s lead with the routine introduction of puberty blockers, which they erroneously describe as “fully reversible” and “provide breathing space to explore options”. See the presentation by Dr Gordon Wilkinson, Sandyford (and page 5 of the Sandyford brochure) which confirms children who are just beginning puberty are now eligible for blockers (so long as they persistently like the stereotypes associated with the opposite sex).
The research which formed the basis of the Gender Identity Service’s extension in the standard use of puberty blockers is flawed in that it had no control group and inaccurately reported positive results, when in fact the preliminary data suggested an increase in behavioural and emotional problems after treatment for one year, a significant increase in reported self-harm and no significant changes in gender dysphoria.
Increasingly doctors and detransitioners are coming forward with concerns about puberty blockers and the impossibility to obtain real informed consent from children about drugs which are being used off-label and with no long-term research into their efficacy. Increasingly evidence is suggesting long-term harm in brain and bone development and significant increased cardiovascular risk. See the current fundraiser for legal proceedings against the NHS.
The recent Health Research Authority review has clarified that puberty blockers are really the start of irreversible physical transition and recommends that “Researchers and clinical staff should consider carefully the terms that they use in describing treatments e.g. avoid referring to puberty suppression as providing a ‘breathing space’, to avoid risk of misunderstanding.”
The situation is compounded by the Memorandum of Understanding, which NHS Scotland signed in Oct 2017, which compels an affirmation only response to children’s statements of believing themselves to be the opposite sex. Fully exploring why a patient holds this belief now leaves health professionals open to accusations of conversion therapy. Point 22 of the MoU requires it to be reviewed after a year, but it is unknown whether this has been carried out; certainly no updated version has been published.
Comment:
We are shocked to learn that routine use of the experimental puberty blockers on an increasing number of young children has seemingly been adopted in Scotland when the evidence for their use points towards severe health issues, and the data for overall use does not appear to be monitored. Given recent events at England’s Tavistock clinic, including clinical whistleblowers and proposed legal action by a concerned parent, we call on the Scottish Government to stop this medical experiment on our children. An inquiry into children’s rights, consent and medical transitioning which has permanent effects, versus the previously recommended ‘watchful waiting’ and unbiased psychological support is urgently needed.
Update 27 March 2021
We have been informed of another Freedom of Information request which gives conflicting information. This FoI from November 2020 gives the following number of referrals:
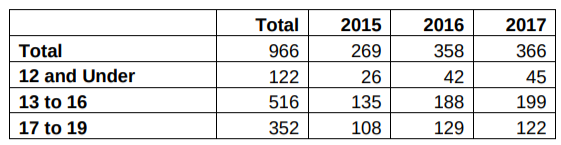
Greater Glasgow and Clyde Health Board stated there were 161 children aged 16 and under who were referred to Sandyford in 2015, 230 in 2016 and 244 in 2017. However, this contradicts the information given to us previously in the FoI from September 2019 (as discussed above) which gave lower figures for each of these years for a wider range of age of children referred to the clinic:
More specifically, we were told there were 181 children aged 13-16 referred to Sandyford in 2017, yet the newer FoI states there were 199.
In the recent Bell v Tavistock court case the children’s gender identity clinic at Tavistock, London was criticised for its poor data collection and analysis. We have previously pointed out that Sandyford is even worse, not even keeping records on the number of referrals for girls, compared to the number of boys. The disparity in even the basic total of child referrals in these FoIs indicates a particularly poor level of record keeping.
Update 28 March 2021:
We submitted a further Freedom of Information request for emails between the Scottish Government and Greater Glasgow and Clyde Health Board regarding puberty blockers after it was revealed that the Scottish Government did not plan to follow the decision of the English courts that puberty blockers could only be prescribed with a court order as children were unlikely to have the capacity to consent to such experimental medication.
The response revealed that the Health Board “can confirm that we have no plans to make any immediate service changes on the back of the recent English High Court ruling” and that there is no minimum age for consideration of prescribing puberty blockers.
It also shows that as early as January 2017, the NHS recognised that the long-term impacts of puberty blockers were not known but could affect bone density and stunt growth. Despite this, a leaflet published by the health board until last year said that taking blockers was considered “fully reversible”.
This has been reported in an article in the Times.
Update 28 November 2021:
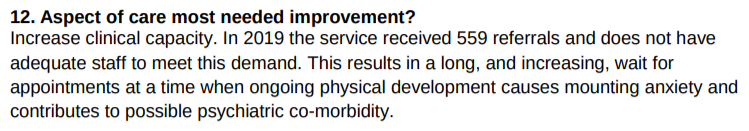
The Service Mapping Report states that the number of referrals to Sandyford’s Young People’s Gender Clinic significantly increased to 559 in 2019.